A thin endometrium can be a silent barrier to conception. This condition affects many women trying to get pregnant but often goes undetected until fertility evaluations begin. Understanding what causes a thin endometrium, recognizing its symptoms and exploring treatment options can help restore reproductive health and improve fertility outcomes.
What is Thin Endometrium?
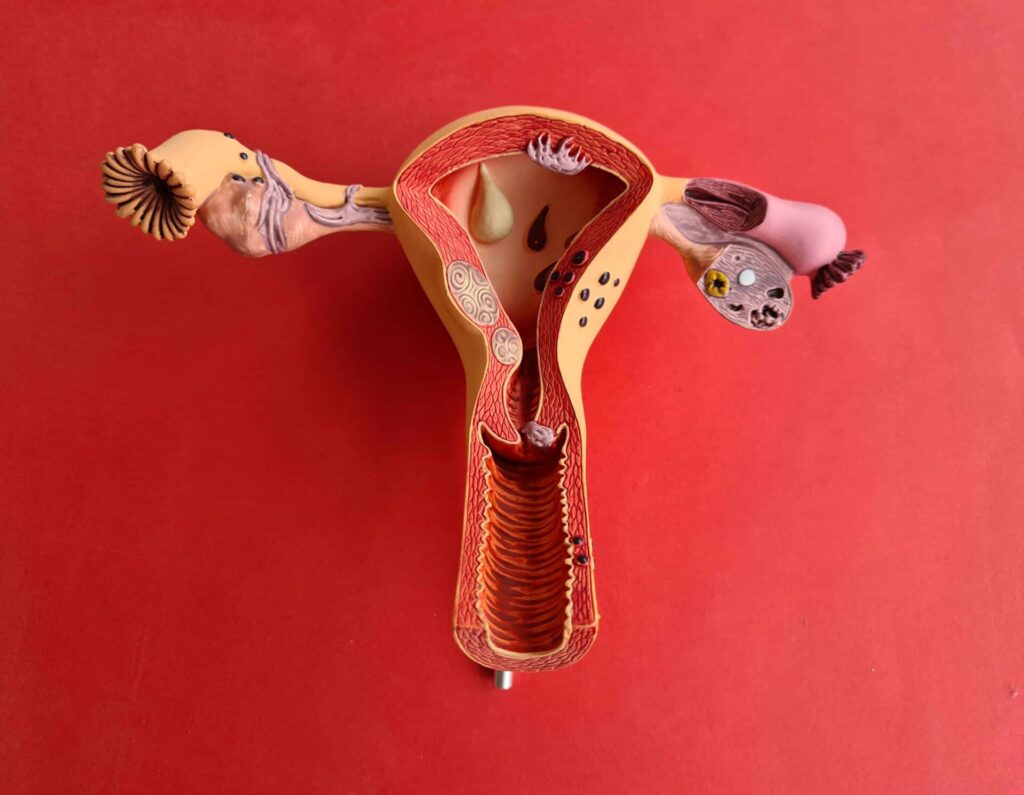
The endometrium is the inner lining of the uterus that thickens each month to prepare for possible embryo implantation. A thin endometrium refers to an endometrial thickness of less than 7mm during the mid-cycle (ovulatory phase), which is typically considered suboptimal for embryo implantation and successful pregnancy.
Causes of Thin Endometrium
A thin endometrium can result from various factors, including hormonal imbalances, medical treatments or lifestyle issues. Below are the most common causes:
1. Low Estrogen Levels
Estrogen plays a crucial role in the development of the endometrial lining. If estrogen levels are too low, the endometrium may fail to thicken adequately.
- Polycystic Ovary Syndrome (PCOS) or premature ovarian failure can lead to hormonal deficiencies.
- Menopausal women naturally produce less estrogen, increasing the risk of a thin endometrium.
2. Uterine Infections or Inflammation
Chronic uterine infections like endometritis can damage the uterine lining and affect its ability to regenerate each cycle.
3. Asherman’s Syndrome
This rare but serious condition involves the formation of scar tissue inside the uterus, often after surgery such as:
- Dilation and curettage (D&C)
- C-section
- Fibroid removal surgery
4. Poor Blood Flow to the Uterus
If the uterus doesn’t receive enough blood, the endometrium may not thicken properly. Contributing factors may include:
- Uterine fibroids
- Pelvic surgery
- Smoking and a sedentary lifestyle

5. Prolonged Use of Hormonal Medications
Long-term use of hormonal contraceptives or fertility drugs like Clomid may impair endometrial growth over time.
Symptoms of Thin Endometrium
A thin endometrium often doesn’t cause noticeable symptoms until fertility is affected. However, some signs can offer early clues:
Common Symptoms
- Irregular or light menstrual periods
- Short menstrual cycles
- Difficulty conceiving
- Early pregnancy loss
Diagnostic Tools
Doctors may use the following methods to diagnose a thin endometrium:
- Transvaginal Ultrasound: Measures endometrial thickness during the menstrual cycle.
- Hysteroscopy: Visualizes the uterine lining and detects adhesions or abnormalities within the uterus.
- Hormonal Tests: Assesses estrogen and progesterone levels.
Why Endometrial Thickness Matters
The thickness of the endometrium plays a crucial role in implantation and maintaining pregnancy. For successful implantation:
- The ideal endometrial thickness is between 8mm to 14mm during the luteal phase.
- A thin endometrium reduces the likelihood of embryo attachment, even in IVF cycles.
Thin Endometrium and IVF
Women undergoing in vitro fertilization (IVF) may have their cycles cancelled or embryos frozen if the endometrium is too thin to support implantation.
Treatment Options for Thin Endometrium
The good news is that thin endometrium can often be treated. Treatment depends on the underlying cause and the patient’s overall health condition.
Estrogen Therapy
Estrogen supplementation is one of the most common and effective treatments.
- Oral Estrogen: Tablets like estradiol increase estrogen levels.
- Transdermal Patches or Injections: For women who can’t absorb oral medications efficiently.
Vitamin E and L-arginine
These supplements are known to improve uterine blood flow, which in turn helps to thicken the endometrial lining.
- Vitamin E: 600 IU/day
- L-Arginine: 6g/day (under medical supervision)
Platelet-Rich Plasma (PRP) Therapy
A cutting-edge treatment involving the infusion of platelet-rich plasma into the uterus to stimulate tissue regeneration and improve thickness.
Acupuncture and Chinese Medicine
Traditional Chinese medicine and acupuncture have shown success in:
- Enhancing uterine blood flow
- Balancing hormones
- Supporting endometrial development
Hysteroscopic Surgery
If adhesions (Asherman’s Syndrome) are the cause, surgical removal of scar tissue can restore the typical endometrial environment.
Lifestyle Changes
Certain habits significantly impact uterine health. To support endometrial growth:
- Quit smoking
- Exercise moderately
- Eat a balanced diet rich in iron, folate and omega-3
- Stay hydrated
Natural Ways to Improve Thin Endometrium
Some women opt for natural remedies in conjunction with medical treatments to enhance their results.
Foods to Include:
- Beets and leafy greens: Boost nitric oxide and improve blood flow
- Pomegranate juice: Rich in antioxidants
- Flax seeds and walnuts: Omega-3 fatty acids for hormonal balance
Yoga Poses for Fertility:
- Cobra pose (Bhujangasana)
- Bridge pose (Setu Bandhasana)
- Legs up the wall (Viparita Karani)
These postures enhance pelvic circulation and reduce stress.
Can You Get Pregnant with a Thin Endometrium?
Yes, some women with a thin endometrium can get pregnant, but the chances may be lower. IVF success rates and natural conception are both influenced by the quality of the endometrial lining.
Tip: Before trying advanced fertility treatments, it’s crucial to address any issues related to thin endometrium to improve pregnancy outcomes.
When to See a Doctor
If you’ve been trying to conceive for 6–12 months without success or have noticed irregular periods or very light menstrual flow, consult a fertility specialist. Early diagnosis of a thin endometrium provides a better chance of effective treatment and conception.
At Boon IVF, Hyderabad, we specialize in diagnosing and treating thin endometrium with a combination of advanced fertility treatments and compassionate care. Our expert team offers personalized solutions—from hormone therapy to regenerative procedures—to help improve endometrial thickness and enhance your chances of conception. If you’re facing fertility challenges related to a thin endometrium, schedule a consultation with our specialists for a thorough evaluation and targeted treatment plan.
Conclusion
A thin endometrium can pose challenges, but with the correct diagnosis and treatment plan, it is often manageable. Whether through hormonal therapy, natural remedies, or advanced medical procedures, women have a range of options to improve their endometrial health and fertility. Prioritizing uterine health and working closely with a fertility expert can make all the difference on your journey to parenthood.


